You can read Part I of my Mastectomy journey here and tips on preparing for a mastectomy here.
I thought I was ready. I thought I was preparing. Having already went through my first mastectomy in August, I thought I knew what to expect. Sure I had some anxiety leading up to the surgery, but overall I thought it was be easier the second time around. Though I would be having the spacers inserted (the first stage of reconstructive surgery), I thought it would be quite similar. I found peace in the low statistical possibility of the same complications that I dealt with in August happening again. My friends and family kept reassuring me that all would go smoothly and I believed them. I could not have been more wrong.
The morning of the surgery, we woke up early, our bags packed and ready to go. We felt experienced, going through the motions. We knew what to bring, where to go and what to expect. We hoped to be back home in 24 hours.
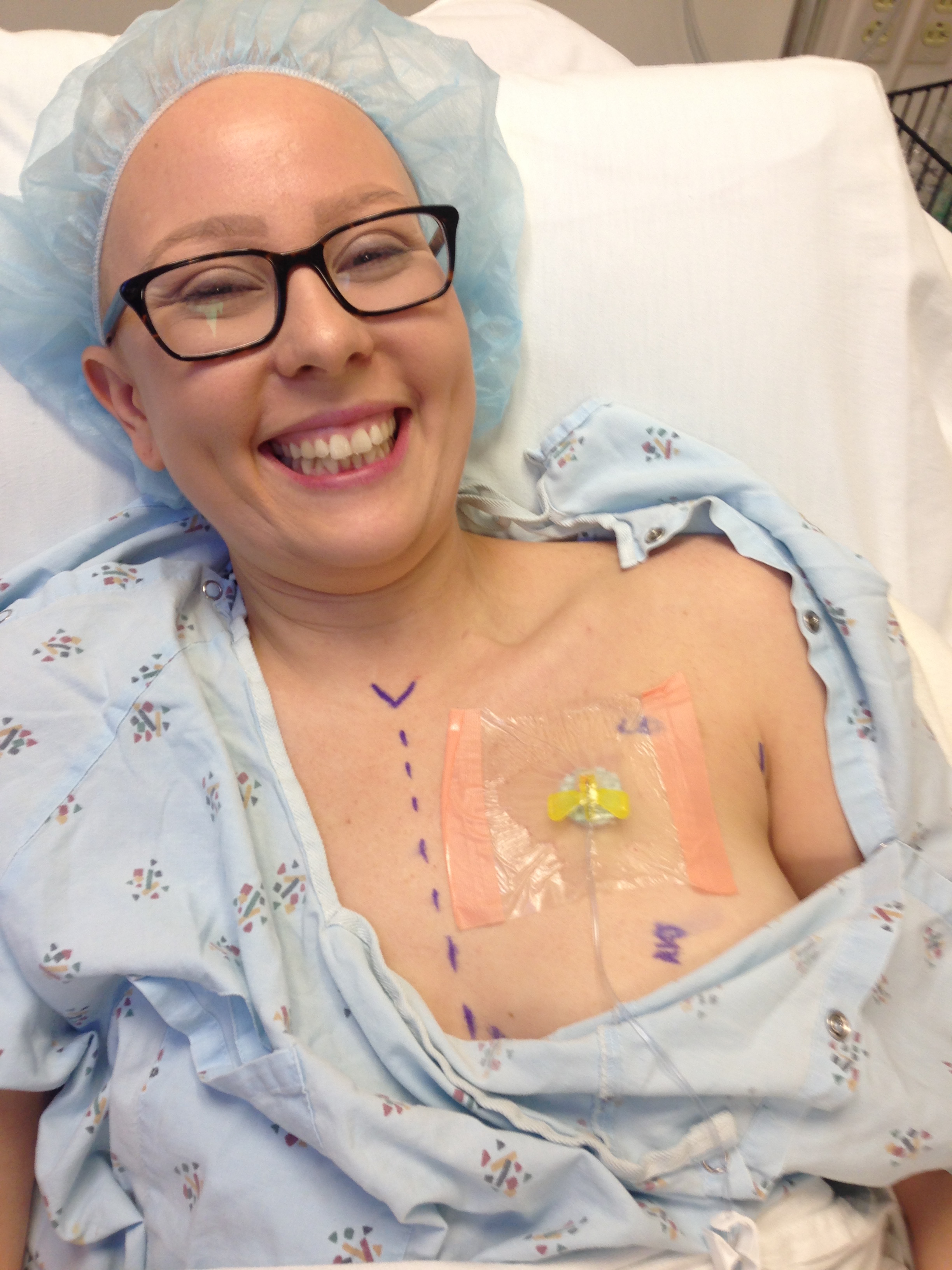
My surgery was scheduled for 8am and the nurses and doctors buzzed around getting everything ready. I changed into my fashionable hospital gown and mushroom hair cap ready to get the surgery over and done with. There was some discussion about removing my port during surgery as it might get in the way, but I pushed to keep it in place. I need the port for the next 6 months of Herceptin infusions. Before I knew it, goofy pictures were taken, loving words were exchanged and the delightful anesthesia cocktail knocked me out.
The following memories are fuzzy. I can’t place the details, the time or the place. I am floating in and out of consciousness, I am freezing and the pain is horrendous. I can’t keep my eyes open like weights are pushing against my eyelids. Later, I would find out my surgery finished early, but there were immediate signs that something wasn’t right. My husband and my mom were left outside for quite a while before being to lead back to my recovery room. When they got there, there were signs that the nurses had struggled to get me to a stable point. Multiple IV lines, and a loose oxygen mask lay on the bed. The vitals machine was flashing showing problematic blood pressure and heart rate readings. Writing these details now as relayed to me second hand, my heart races with fear. I am relieved to have no memory of this time and my heart aches for my mom and Mac who must have been overcome with concern.
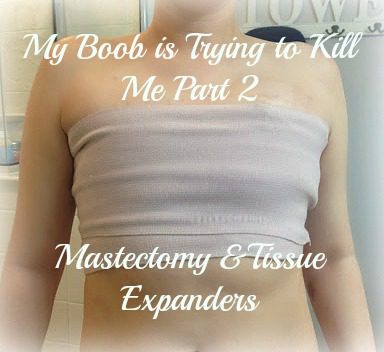
The uncertainty continued. Frustration and concern mounted as the nurses struggled to get me to a manageable pain level, the checkpoint for release to my overnight room. I continued to drift in and out of awareness. I vaguely remember the smiles from some of the familiar nurses and the concerned looks from my surgeons as they hustled in and out. My bandages were removed, revealing an excessive amount of bruising and swelling.*Warning: The images below may be disturbing. Proceed with caution. Mac pushed the nurses to get the doctors. The swelling was much worse than my hematoma in August and Mac now knew the warning signs to look for. Without hesitation, my surgeons made a quick decision to return to the OR. All I could think about was getting the huge elephant off my chest — the pressure was unbearable.
It’s hard to believe that this photo was after my mastectomy. It looks like there is still breast tissue in there, but that is all swelling due to the excess fluid.
The doctors and nurses worked with precision and speed to get the problem resolved. When they opened my chest back up, they found that a spot under the port flap had begun to bleed after they closed me up. The fluid and blood had begun to build up under my skin causing the swelling. After they removed 600mL of fluid and blood, they cauterized “the bleeder”. They also had to pump my stomach to remove a large bubble of air the size of a grapefruit, which had resulted during anesthesia. Additionally, the doctors removed 800 mL of urine from my bladder and put in a catheter. They ended my second surgery with external stitches on the problematic side, unlike the internal dissolvable stitches used before.
The next thing I remember is waking in the recovery room for the second time with the same friendly nurses by my side. The pain was still coursing through me and the anesthesia jumbled my thoughts. I saw Mac and my mom come in and I heard far off voices discussing the next steps. They needed to move me from the ACC to the main hospital in order to have me monitored over night. Though the distance was less than a block between buildings, the only way to get me there was an ambulance (woohoo, my first ambulance ride). I was still in a daze just floating along as they wheeled me through the hospital. I could feel the pain with every bump and movement, but the weight on my eyelids kept me from opening my eyes.
The next few days were a haze of pain and sleep. I would wake for short periods of time to take more pain medicine and administer my vitals. I was poked and prodded constantly for 3 days (7 different needle sticks – not to mention the 2 sticks to retrieve arterial blood. One stick in each wrist and some “searching” for the artery). Luckily the second surgery had resolved the hematoma but that additional surgery left my body extremely traumatized. The blood I had lost impacted my energy and I had no appetite. Tons of painkillers on an empty stomach are not a combination for success. I was receiving IV Dilaudid, Morphine and Fentanyl in addition to the tablets of Hydrocodone and Dilaudid. The pain was unlike anything I’d ever felt before. Thinking back to my first surgery, I thought I would know this pain and be able to handle it better. Boy, was I wrong. It felt like a huge elephant was sitting on my chest. The pressure was unbearable. Any slight movement sent currents of pain surging through my chest muscles. I had three surgical JP drains to route fluid out of my body. Two were under the chest muscles and one was on top of the muscle near the hematoma site. The drains use suction to remove any fluid or additional bleeding. Every time the drained were stripped or “milked” I could feel the suction inside of my body like a straw trying to suck a chunk of ice from a milkshake. This sensation was unlike anything I’d ever felt. Imagine someone took a straw inserted into your chest and began sucking. As the suction searches for liquid, you feel the painful pull against your dry muscles, tissue and nerves.
I was scared. I didn’t feel like myself and I this pain was so new and overwhelming it terrified me. I felt like it would never end, I kept waiting to wake up from a bad dream. I went in feeling so prepared and so close to the end that this contrasting reality hit me hard. I wasn’t strong enough or awake enough to have visitors and I could barely muster the energy to respond to the doctors questioning. The doctors kept telling me the pain was normal due to the tissues expanders and the cuts to my chest muscles. Their reassurances of normality did nothing to subdue my fears and suffering.
I couldn’t do anything by myself. I felt trapped. I couldn’t get out of bed on my own. I couldn’t use the bathroom on my own. I had a catheter for two days and even my bladder had forgotten how to work. Imagine your arms are strapped to your sides and you can’t use your chest muscles at all, shoulders or arms at all. That will give you a sense for my limitations. It was a group effort to get me out of bed and to the bathroom. Luckily I was so constipated from the pain meds I didn’t have to have someone wipe my butt. These physical limitations were exhausting and frustrating.
The nurses wanted me up and moving as much as possible, but all I wanted to do was sleep. My eyelids were heavy and I could barely stand up — the pain was too much. Walking felt like a nightmare. Mac and my mom pushed me though and I made it out into the hallway two times a day. I must have been a sight to see. Draped in two hospital gowns to cover my bright white butt, I struggled down the hallway at a snail’s pace. Each lap around the unit is 1/17th of a mile. I couldn’t even make it around once. My legs would give out and with each step the pain in my chest multiplied.
On Thursday, the doctors decided to give me a blood transfusion, another first for me. My blood levels were very low due to the blood I lost in surgery. My face was white and skin showed a greenish/yellow tinge. Deep dark circles surrounded my eyes. The hope was that the transfusion would bring me back to life.
As if the pain, constipation, fatigue and stomach discomfort weren’t enough, I also developed a heat rash all over my chest, shoulders and neck. It felt like chicken pox. The desire to scratch my skin for relief was uncontrollable. The bandages and compression materials that touched my skin caused immediate irritation. I was covered in bruises from the IVs sticks and examinations. Benadryl and hydrocortisone cream brought me some relief but the urge to itch my skin is still driving me insane. I can’t shower until all my drains are removed, which hasn’t helped the state of my irritated skin. I am counting down the days until Thursday.
After my surgery, the hematology team asked me a million questions and analyzed my blood, trying to find an explanation for the second hematoma. Everyone was baffled. It is unlikely to have a hematoma with a mastectomy surgery and here I was having two within a 6-month period. It was especially odd that I have no history of blood clotting problems. For perspective my surgeon has only had one other similar case in over 2o years of experience. There were no conclusive results from the testing, but they want to run more tests on me in the coming weeks to determine a proactive blood clotting medication plan for my next surgery.
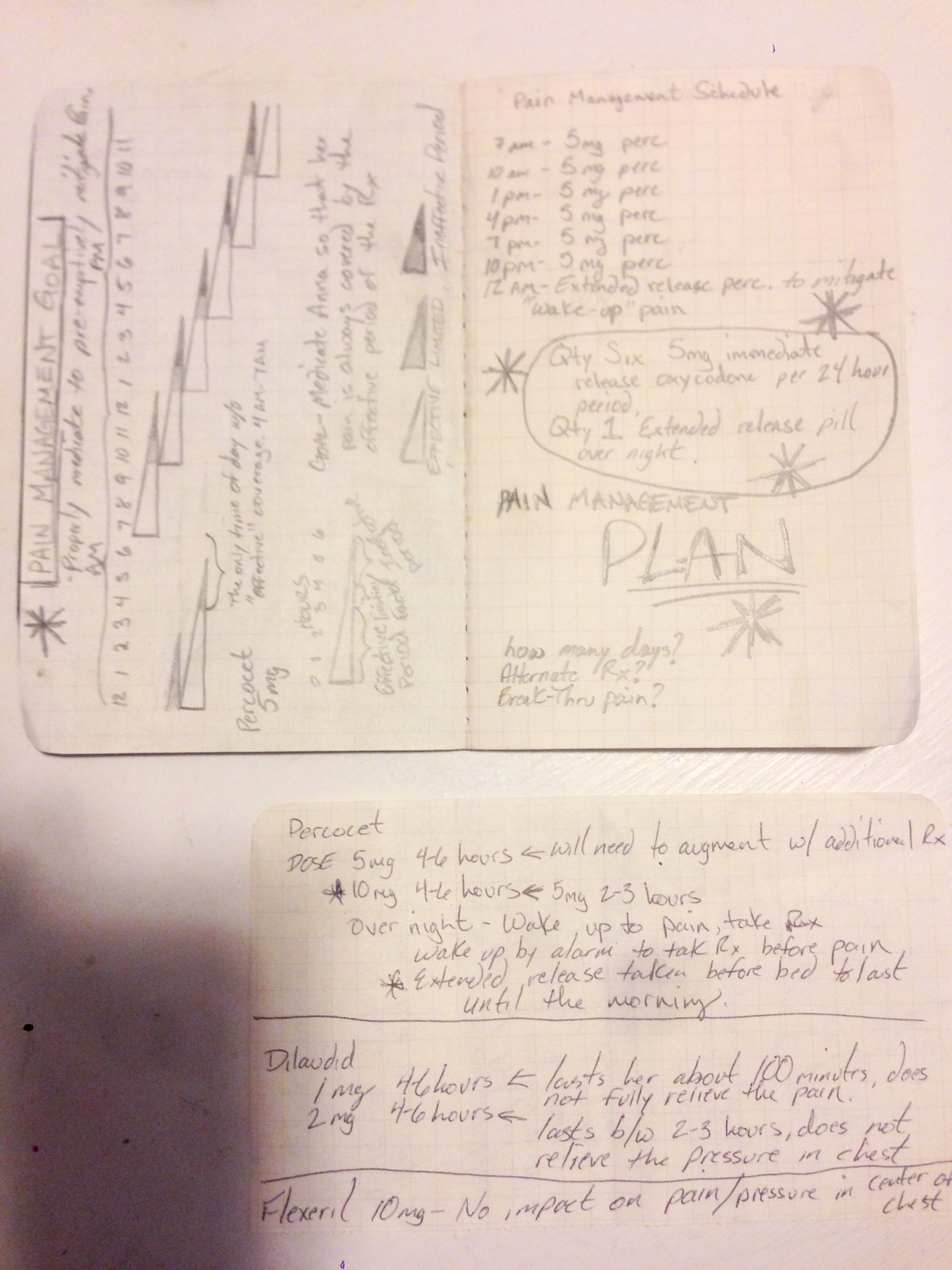
Luckily, the blood infusion helped significantly and the color slowly came back to my face and skin. Though the doctors felt I was stable enough to go home, I was terrified to leave. I didn’t want to leave the security and comfort of the hospital and I really didn’t want to part with the IV pain medication, my only relief. I was still in a lot of pain and the uncertainty of facing the pain and recovery at home without constant check-ins from the nurses and doctors felt overwhelming. After monitoring and tracking my pain medication with extreme detail, Mac devised a new plan for the timing and dosage. He was able to get the doctors and nurses to agree and they were finally able to get me to a consistent and manageable pain level. I have attached an image below of the dosing plan that Mac devised. He will be sharing more documents and templates soon for caregivers to use.
Despite my fears, we were home by Thursday evening, 60 hours after we walked in my surgery. For reference, Mac slept for the first time around 5:45am Wednesday morning. He was so happy to get me home and to finally be able to sleep himself; relieved I was stable showing improvements. For the first couple days at home, I slept nonstop. I still couldn’t get out of bed or up from a chair without assistance. Luckily I have amazing family and friends who helped me get around the house, bathed me, fed me and helped me to the bathroom. It’s not a fun feeling depending on others to complete basic survival tasks. Unfortunately, this is just the reality of recovery. Just say “thank you” to your caregivers and remember that they love you and want to help in any way they can.
Mac built me this amazing table to assist during my recovery. It made life on the couch for days on end much easier.
Little by little my days are getting better and my pain is more manageable. Last Friday, I had 2 of my 3 drains removed, which was extremely exciting. Now I am only hanging on to the one drain, which will be removed this Thursday. I am trying to wean off the pain pills a little at time, but the swelling and inflammation are still present due to the complications during surgery. My mind has recovered quickly and I am ready to get back to normal life, but unfortunately my body isn’t as fast. I am trying to stay positive and demonstrate patience for my body. I have to make it through 4-6 weeks of limitations and recovery. No cooking, cleaning, or lifting. Any deviation from the limitations and requirements could result in movement of the tissue expanders, another surgery and/or extended recovery time.
After I get my final drain removed this week, we will wait one more week for the final healing and then I will begin the tissue expansion process. Every week the plastic surgeon nurse will use a magnetic needle to locate the deflated tissue expander below my pectoral muscle and she will inject it with 30-120mLs of saline. The amount of saline each visit will be dependent on my pain tolerance as the saline stretches my muscle making room for the inflated expander. The weekly process will continue until the expanders have reached the desired size. I know many of you are pushing for “Dolly Partons”, but I think I’ll stick with my pre-cancer size. There will then be a 3 month waiting period, which allows for my to adjust to the pocket size. At the end of the 3-month period, I will go back into surgery to have the inflated tissue expanders switched out for the permanent implants. I am quite nervous about this new stage and the pain and emptions it may bring for me. But like the rest of my journey, I will take it one day at a time. I don’t think anything can be worse than the pain I have experienced these past few weeks and each day brings me one step closer to the end of this cancer recovery process.
So you may be wondering, why would I go through this horrendous process again if my cancer was removed during the first mastectomy? I decided to go through of this to be proactive about my care and well-being. Making this decision allowed me to take control of my life. I want to know that I did everything I possibly could to eliminate my risk of future reoccurrence. I don’t want to look back and have regrets or worry that I could have done more to prepare myself for the future. Each year I want to be celebrating the diminishing probability that breast cancer will return. Without removing the other breast I would be wondering more and more each year if breast cancer would attack me again. I felt it would be like choosing to keep a ticking time bomb. I want to live a long life free of fear and these decisions are my first steps in that direction. I want to rebuild and strengthen this body of mine. This poor body that has been attacked and mutilated. The second mastectomy and my reconstruction bring me closer to feeling whole again. In these moments of pain, despair and sadness, I try to look forward to the new stronger me that is waiting on the other side. I am almost there, only 7 months to go!
*Side note, if you want a brow product that will last through surgery and days of recovery, get the new Brow Definer Pencil from Anastasia Beverly Hills. That pencil is magic. This has been especially helpful for me right now since my eyebrows decided to fall out now, a month and a half after chemo ended.





29 Comments